Contact us
Precision Medicine
What is tachycardia?
25 September 2025
Tachycardia is an abnormality where a person’s heart rate is faster than normal while at rest, exceeding 100 beats per minute. A normal heart rate is typically between 60 and 100 beats per minute.
With tachycardia, the heart is forced to overwork as it has to pump blood faster. If not diagnosed and treated in time, it can lead to a stroke (cerebrovascular event), heart failure, or a heart attack, which can leave a person with lasting health problems or even be fatal.
Causes of Tachycardia
This condition is due to an alteration in the heart’s electrical impulses, caused by any of the following factors:
- Congenital heart abnormalities.
- Excessive use of tobacco, coffee, drugs, or alcohol.
- Electrolyte imbalance.
- Heart or lung diseases.
- Stress.
- Hypertension.
- Hyperthyroidism.
- Reaction to certain medications.
Sometimes, it’s not possible to identify the cause of the tachycardia, but some genetic inheritance factors can contribute to its onset.
There are several types of tachycardia, including:
- Atrial flutter: The atrium beats fast but regularly.
- Atrial fibrillation: This is the most common type and involves an increase in the heart’s electrical activity, leading to irregular heartbeats.
- Ventricular fibrillation: This occurs during or after a heart attack. Here, the ventricles move chaotically instead of pumping blood. If not immediately regulated, it can cause death.
- Supraventricular tachycardias: This is usually due to a congenital heart defect.
- Ventricular tachycardias: This results in an insufficient blood supply to the body.
Signs and symptoms Tachycardia
Although tachycardia can be asymptomatic in many cases, some people may experience symptoms that affect their well-being and quality of life. Identifying these symptoms is crucial to determine the severity of the episode and seek timely medical attention. The most common symptoms include:
- Dizziness, lightheadedness, and confusion.
- Weakness.
- Loss of consciousness.
- Chest tightness and pain.
- Difficulty breathing.
- Episodes of fast or irregular palpitations.
- Rapid pulse.
Tachycardia can lead to serious, life-threatening complications.
Diagnosis Tachycardia
The diagnosis of tachycardia begins with a detailed clinical evaluation, where the doctor gathers information about the patient’s symptoms, their frequency, duration, and any known triggering factors.
In addition, a physical exam should be performed to measure heart rate and blood pressure, and to look for signs that might indicate a possible underlying cause, such as heart murmurs, paleness, or excessive sweating.
It is necessary to inquire about the patient’s and their family’s medical history, as some forms of tachycardia may be related to genetic predisposition or pre-existing diseases such as hypertension, thyroid disorders, or heart failure.
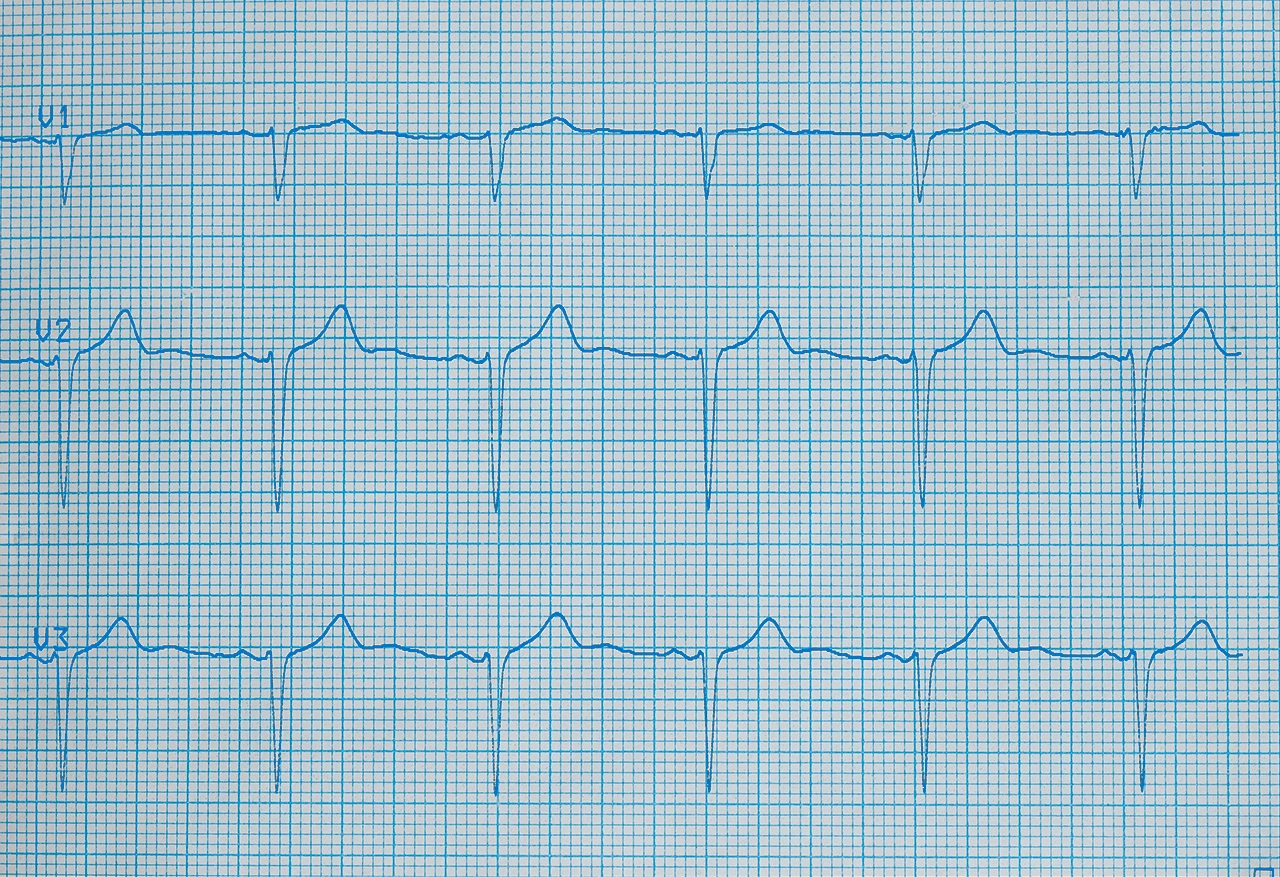
To confirm the diagnosis and determine the specific type of tachycardia, complementary studies are used, such as an electrocardiogram (ECG), which analyzes the heart’s electrical activity at rest.
A 24- to 48-hour Holter monitor may be required in cases where the episodes are intermittent; this device records heart activity over prolonged periods.
Stress tests, echocardiograms, or electrophysiological studies may be necessary to identify structural abnormalities or changes in the heart’s electrical conduction, providing key information for giving the proper treatment.
Treatment Tachycardia
Depending on the underlying cause of the tachycardia, its frequency, the duration of the episodes, and the impact it has on the patient’s health, the most appropriate treatment must be chosen.
In mild or episodic cases, only lifestyle changes may be recommended, such as reducing caffeine, alcohol, or tobacco consumption. Regular exercise and stress management techniques may also be advised.
For cases where there is a greater impact on the person’s health, pharmacological treatment such as beta-blockers or calcium channel blockers may be needed to help regulate the heart rate.
In more severe cases, medical procedures like electrical cardioversion or catheter ablation can be used. The implantation of an automatic defibrillator may be indicated for patients at risk of dangerous arrhythmias.
It is important to see a specialist not only to treat the tachycardia but also to understand its origin and address its cause.
Preventing Tachycardia
It is possible to prevent tachycardia by modifying habits to lead a healthy lifestyle:
- Avoid being overweight and obese.
- Relax and try to eliminate your sources of stress or your response to them.
- Maintain a diet that avoids fats, sugars, and processed foods, prioritizing fiber and vegetables.
- Exercise regularly.
- Avoid smoking, alcoholism, and high coffee consumption.
- Control your blood pressure.
- Do not self-medicate.
Contact the Arrhythmia Clinic at Centro Médico ABC for specialized care!
Fuentes:
How can we help you?

Ricardo Ostos
Content CreatorLearn more about Ricardo on LinkedIn