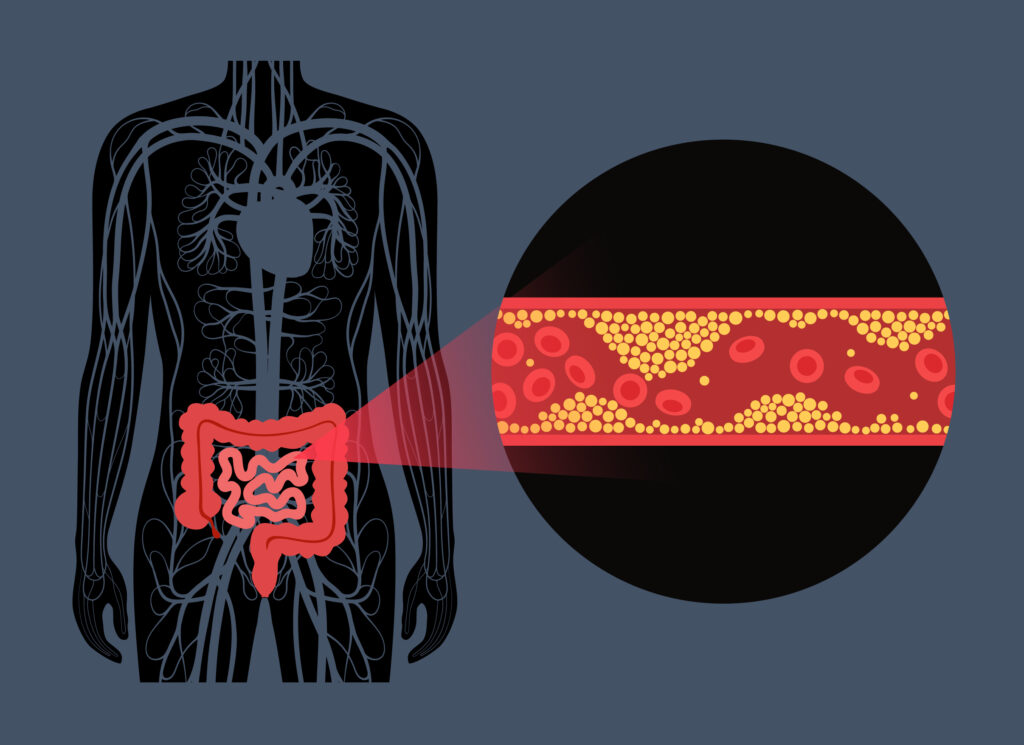
What is mesenteric venous thrombosis?
Mesenteric venous thrombosis refers to the occlusion of the veins that drain blood from the intestines. This obstruction causes an increase in the pressure of the intestinal wall, which causes ischemia (lack of blood). Ischemia is caused when the arteries that go to the intestine cannot overcome the pressure therein, thus blocking the arterial circulation that carries oxygen and nutrients.
Mesenteric venous thrombosis can be acute, subacute, or chronic. It usually affects the distal small intestine, rarely involving the colon.
The accumulation of liquids in the intestinal wall and within the intestinal lumen produces hypovolemia, which decreases the blood supply, thus increasing intestinal ischemia. All this is also aggravated by the vasospasm produced by venous thrombosis and intestinal edema.
Mesenteric Venous Thrombosis- Risk Factors
Mesenteric venous thrombosis is considered a multifactorial disorder, and they are divided into acquired or hereditary factors.
Intra-abdominal inflammatory processes are important risk factors: pancreatitis, intestinal inflammation, trauma (splenectomy), weight loss laparoscopic surgeries, etc.
Acquired or hereditary thrombophilia, such as prothrombin gene mutations (G20210A), nephrotic syndrome, cancer, etc.
Acute respiratory syndrome due to infection with coronavirus 2 is also related to mesenteric vein thrombosis.
Other causes are abdominal masses that cause venous compression, myeloproliferative disorders, portal hypertension and cirrhosis, history of deep venous thrombosis.
Mesenteric Venous Thrombosis- Signs and Symptoms
The age at which it occurs most frequently is between 45 and 60 years. With a slight male predominance.
Acute: it begins with cramping pain around the navel, which lasts for hours and is unrelated to the abdominal physical examination, which is almost normal. Sometimes the pain does not start so abruptly and is usually dull and insidious. The symptoms usually last from 5 to 14 days before going to the doctor. Nausea and/or vomiting may appear.
Abdominal distention may occur. Alarm data is usually seen when the thrombosis is very advanced.
X-rays do not usually help much in this state.
Subacute: Symptoms appear for days to weeks before diagnosis. The most common sign, and many times the only one, is non-specific abdominal pain. This occurs in patients with partial or distal thrombosis that develop new collaterals.
Chronic: These patients are usually asymptomatic. The diagnosis is made incidentally. When these patients have symptoms, they are rather related to portal hypertension (varices and esophageal bleeding). Few patients have abdominal pain after eating.
Mesenteric venous thrombosis – Diagnosis
There are no clinical or laboratory characteristics that establish the diagnosis.
Half of the patients have a personal or family history of deep vein thrombosis or pulmonary thromboembolism.
The definitive diagnosis is established with imaging studies that verify thrombosis in the mesenteric veins. This is accomplished with magnetic resonance venography or late-phase venous contrast-enhanced and non-contrast CT. When these tests are not conclusive, venography with intravenous catheters is used.
Once the diagnosis of mesenteric venous thrombosis has been established, thrombophilia (genetic or acquired) must be ruled out.
Mesenteric Venous Thrombosis – Treatment
It is primarily conservative, with anticoagulation to stop thrombus spread, fasting to rest the bowel and close monitoring for complications. Rehydration is essential. In well-selected patients, clot-dissolving drugs can be used. Surgery is reserved for patients in whom intestinal infarction is confirmed or when it is highly suspected.
Anticoagulation should be given for periods of at least 3 months depending on each case.
At ABC Medical Center’s Cardiovascular Center, we can provide you with specialized care. Contact us!
Fuente:
Dr. Claudio Alberto Ramírez Cerda– Vascular and Endovascular Surgery specialist at ABC Medical Center.