Oncology interventional imaging and radiology
Imaging studies play an essential and growing role in oncology. We have state-of-the-art technology and expert doctors in early detection, diagnostic evaluation, characterization, staging, follow-up, therapeutic response monitoring, and active cancer surveillance.
Various modalities are used, conventional x-rays, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound (US), positron emission tomography (PET), and/or hybrid equipment that provides fused images (PET- CT), depending on the location of the tumor, the stage of the disease, the main purpose of the study, among others.
We offer specialized high-resolution technology for breast cancer evaluation, such as Digital Mammography. And for prostate cancer, Prostatic Multiparameter Magnetic Resonance (pmMRI), an advanced technique for the detailed characterization of lesions and therapeutic decision-making, for example, helping to distinguish those that require treatment from those that can be followed with active surveillance.
Our Interventional Radiologists perform minimally invasive procedures guided by real time images, both diagnostic (biopsies) and therapeutic (ablation), with great precision. Image-guided biopsies seek to define the exact location of the tumor lesion and obtain an optimal tumor tissue sample for histopathological diagnosis and/or molecular analysis. Radiofrequency, microwave, or freezing ablation is intended to destroy the tumor without removing it (the body removes the dead tumor tissue leaving a scar), that is, without the need for surgery.
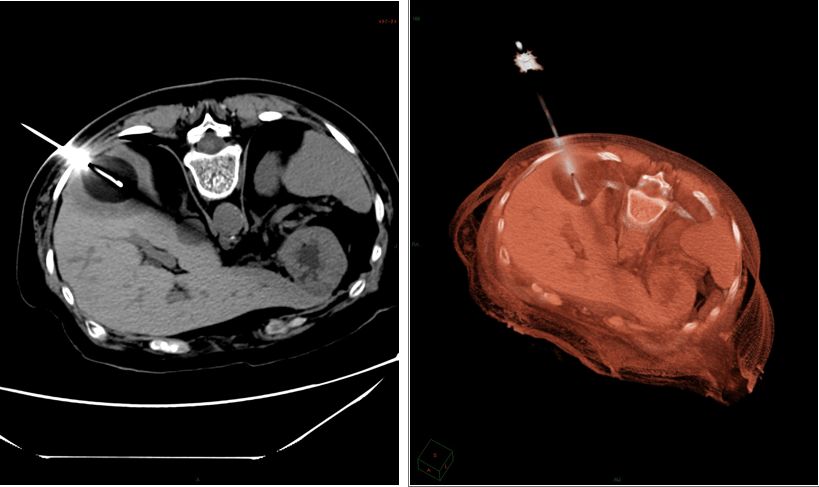
Cryoablation of liver metastases
The interventional radiologist uses real-time imaging to guide a needle / catheter to the tumor lesion.
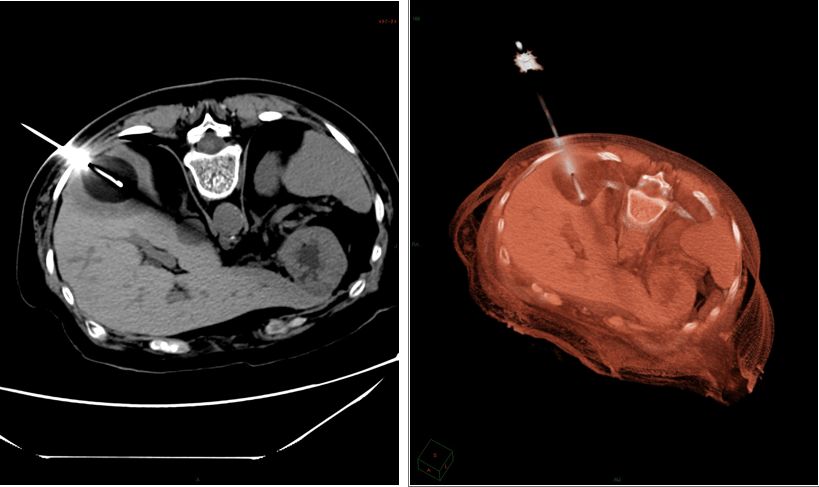
Cryoablation of liver metastases
The interventional radiologist uses real-time imaging to guide a needle / catheter to the tumor lesion.
Nuclear Cancer Medicine
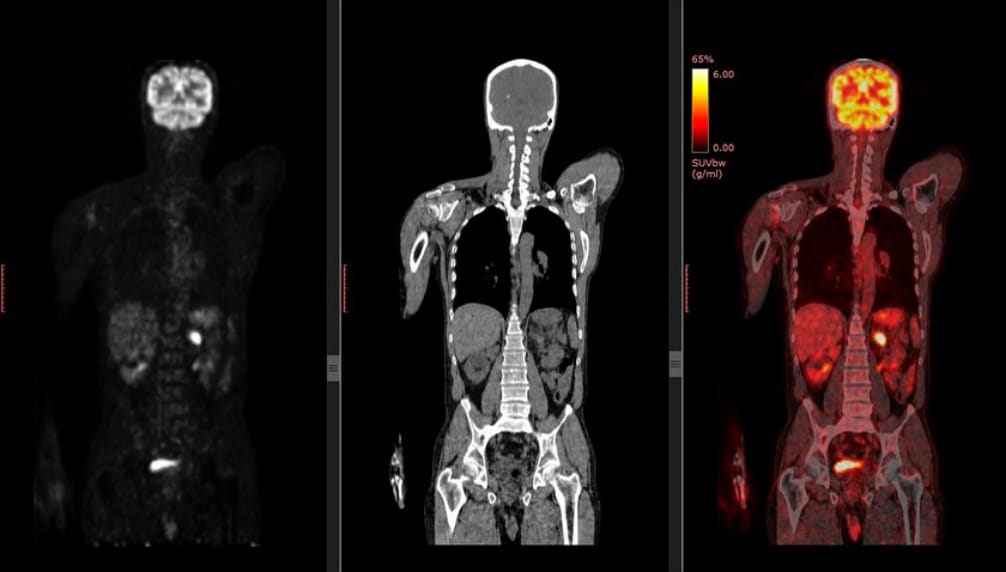
In the field of treatment, we have the latest generation radiopharmaceuticals (drug or carrier molecule linked to a radioactive isotope) to offer you theranostics. Theranostic treatment, a term derived from the combination of ‘therapy’ and ‘diagnosis’, consists of injecting a radio drug [or theranostic agent] in small doses and obtaining an image of the radiopharmaceutical uptake areas corresponding to tumor lesions.
Based on the results of this diagnostic image, and with strict safety guidelines, a higher dose of the radiopharmaceutical (therapeutic radiation dose) is prescribed. Radiation emitted by the radiopharmaceutical within tumor lesions selectively kills cancer cells, minimizing damage to adjacent healthy cells. Several treatment sessions are usually given, monitoring the response with images.
Theranostic has been used for many years in the treatment of certain types of thyroid cancer. Now, the development of novel radiopharmaceuticals is allowing theranostics to offer new possibilities for therapy to a growing number of tumors, including neuroendocrine tumors, neuroblastoma, and prostate cancer.
Therapeutic Nuclear Medicine (Theranostic)
The theranostic agent 77 Lu-PSMA offers a new alternative in the treatment of prostate cancer. PSMA, or prostate specific membrane antigen, is a receptor that is overexpressed in certain types of prostate cancer, being an ideal molecular target for diagnostic-therapeutic purposes for metastatic prostate cancer, and its use is explored in earlier stages of the illness.
Diagnostic and follow-up nuclear medicine
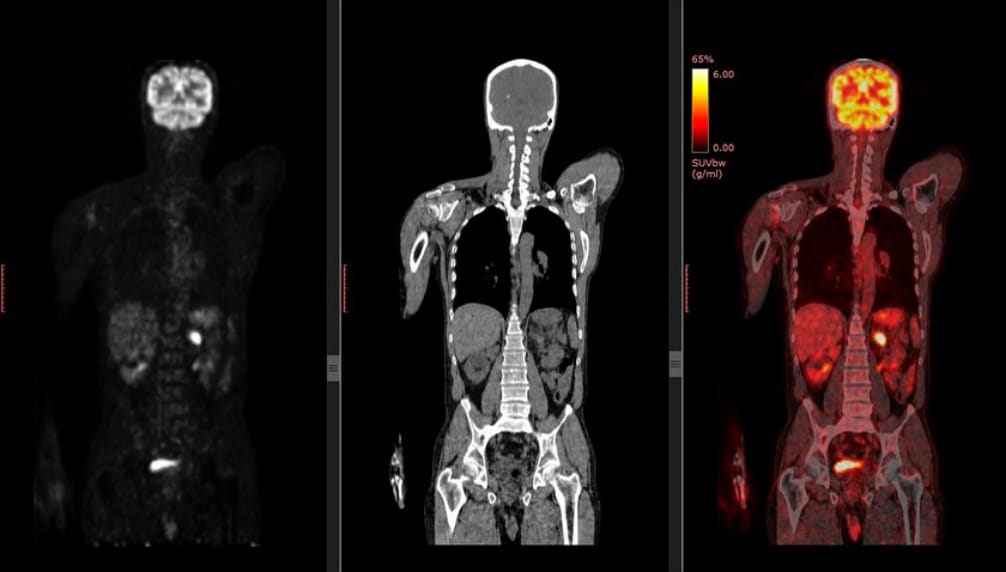
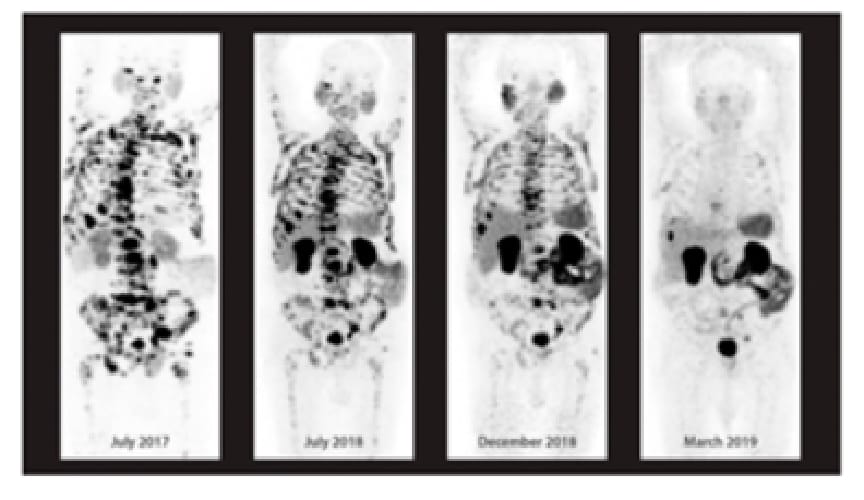
PET provides a total body image for metastasis tracking
The fusion of PET with other imaging studies, PET/CT and/or PET/MRI, helps to determine the anatomical location of tumor lesions.
The F-FDG PET (PET using the Fluorodeoxyglucose radiotracer) allows detecting and measuring tumor metabolic activity due to the high glucose consumption of most neoplastic cells.
With state-of-the-art equipment and next-generation radiotracers and theranostic agents, the ABC Department of Nuclear Medicine offers the latest in cancer diagnosis, monitoring, and treatment.
Through the PET equipment, or positron emission tomography, and through the use of radiotracers or radiopharmaceuticals injected in small doses, the spread of cancer throughout the body is tracked. PET detects non-visible lesions with other imaging studies, managing to identify hidden metastases, more accurate staging, and earlier detection of recurrences. In addition, it provides functional information indicating the degree of tumor activity and response to treatment.
Medicina nuclear oncológica
Diagnostic and follow-up nuclear medicine
PET provides a total body image for metastasis tracking
The fusion of PET with other imaging studies, PET/CT and/or PET/MRI, helps to determine the anatomical location of tumor lesions.
The F-FDG PET (PET using the Fluorodeoxyglucose radiotracer) allows detecting and measuring tumor metabolic activity due to the high glucose consumption of most neoplastic cells.
With state-of-the-art equipment and next-generation radiotracers and theranostic agents, the ABC Department of Nuclear Medicine offers the latest in cancer diagnosis, monitoring, and treatment.
Through the PET equipment, or positron emission tomography, and through the use of radiotracers or radiopharmaceuticals injected in small doses, the spread of cancer throughout the body is tracked. PET detects non-visible lesions with other imaging studies, managing to identify hidden metastases, more accurate staging, and earlier detection of recurrences. In addition, it provides functional information indicating the degree of tumor activity and response to treatment.
Therapeutic Nuclear Medicine (Theranostic)
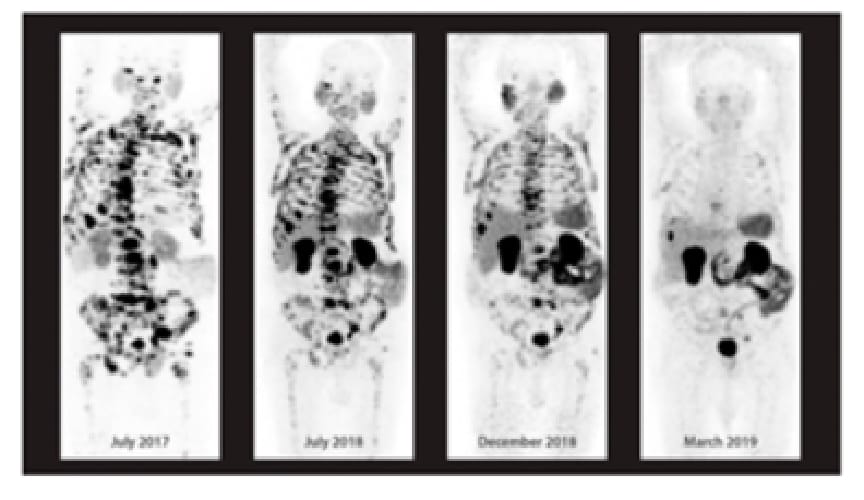
The theranostic agent 77 Lu-PSMA offers a new alternative in the treatment of prostate cancer. PSMA, or prostate specific membrane antigen, is a receptor that is overexpressed in certain types of prostate cancer, being an ideal molecular target for diagnostic-therapeutic purposes for metastatic prostate cancer, and its use is explored in earlier stages of the illness.
In the field of treatment, we have the latest generation radiopharmaceuticals (drug or carrier molecule linked to a radioactive isotope) to offer you theranostics. Theranostic treatment, a term derived from the combination of ‘therapy’ and ‘diagnosis’, consists of injecting a radio drug [or theranostic agent] in small doses and obtaining an image of the radiopharmaceutical uptake areas corresponding to tumor lesions.
Based on the results of this diagnostic image, and with strict safety guidelines, a higher dose of the radiopharmaceutical (therapeutic radiation dose) is prescribed. Radiation emitted by the radiopharmaceutical within tumor lesions selectively kills cancer cells, minimizing damage to adjacent healthy cells. Several treatment sessions are usually given, monitoring the response with images.
Theranostic has been used for many years in the treatment of certain types of thyroid cancer. Now, the development of novel radiopharmaceuticals is allowing theranostics to offer new possibilities for therapy to a growing number of tumors, including neuroendocrine tumors, neuroblastoma, and prostate cancer.
Oncology Precision Medicine Unit
Tumor molecular characterization using next-generation sequencing (NGS) offers new and highly personalized therapeutic options and strategies.
Advances in oncology have made it possible to discover that cancer has a genomic basis. Genomic alterations, or mutations, responsible for the development and growth of many types of cancer are known. This has led to the development of new cancer therapies, innovative drugs directed against these alterations or molecular targets, the so-called ‘targeted therapies’ or ‘target therapies’.
Precision oncology focuses on finding the unique genomic alterations in your cancer and expanding your treatment options by selecting those targeted therapies.
In addition, the evaluation of other characteristics such as the tumor mutational burden (TMB) and/or microsatellite instability can help predict the response to immunotherapies.
The Oncology Precision Medicine Unit is dedicated to bringing advances in genomics to oncology practice at ABC and constantly updating knowledge in this area. We seek alliances with the most important international genomic companies in oncogenomics, not only to offer the most advanced and validated tests to ABC patients, but also to bring the benefit of these companies’ expertise through Molecular Tumor Boards, among other precision oncology platforms.

ABC Cancer Center Molecular Tumor Board
We are the first medical center in Mexico to implement Molecular Tumor Board sessions with molecular experts and international clinical oncologists. It delves into the interpretation of the genomic alterations found and their clinical significance in the patient, recent publications are reviewed, possible targeted therapies and strategic therapeutic combinations are evaluated, eligibility for clinical trials is explored, etc. in search of the best therapeutic options.
ABC Cancer Center
Molecular Tumor Board

We are the first medical center in Mexico to implement Molecular Tumor Board sessions with molecular experts and international clinical oncologists. It delves into the interpretation of the genomic alterations found and their clinical significance in the patient, recent publications are reviewed, possible targeted therapies and strategic therapeutic combinations are evaluated, eligibility for clinical trials is explored, etc. in search of the best therapeutic options.
Tests to know the specific genomic alterations of your cancer.
Although only the most commonly mutated individual genes in the type of cancer can be analyzed, it is preferable to obtain the tumor molecular profile through next generation sequencing panels (NGS), which evaluate hundreds of genes associated with cancer.
Obtaining the tumor’s molecular profile makes it possible to discover other genomic alterations (in addition to those best known for the type of tumor) for which there may be targeted therapies, rule out possible mutations related to resistance to targeted therapies, and search for strategic therapeutic combinations, among other advantages.
Genomic analysis is performed on samples of tumor tissue obtained by biopsy or surgery, and in advanced metastatic stages also on blood samples (so-called “liquid biopsies” or “non-invasive biopsies”).
Liquid Biopsy
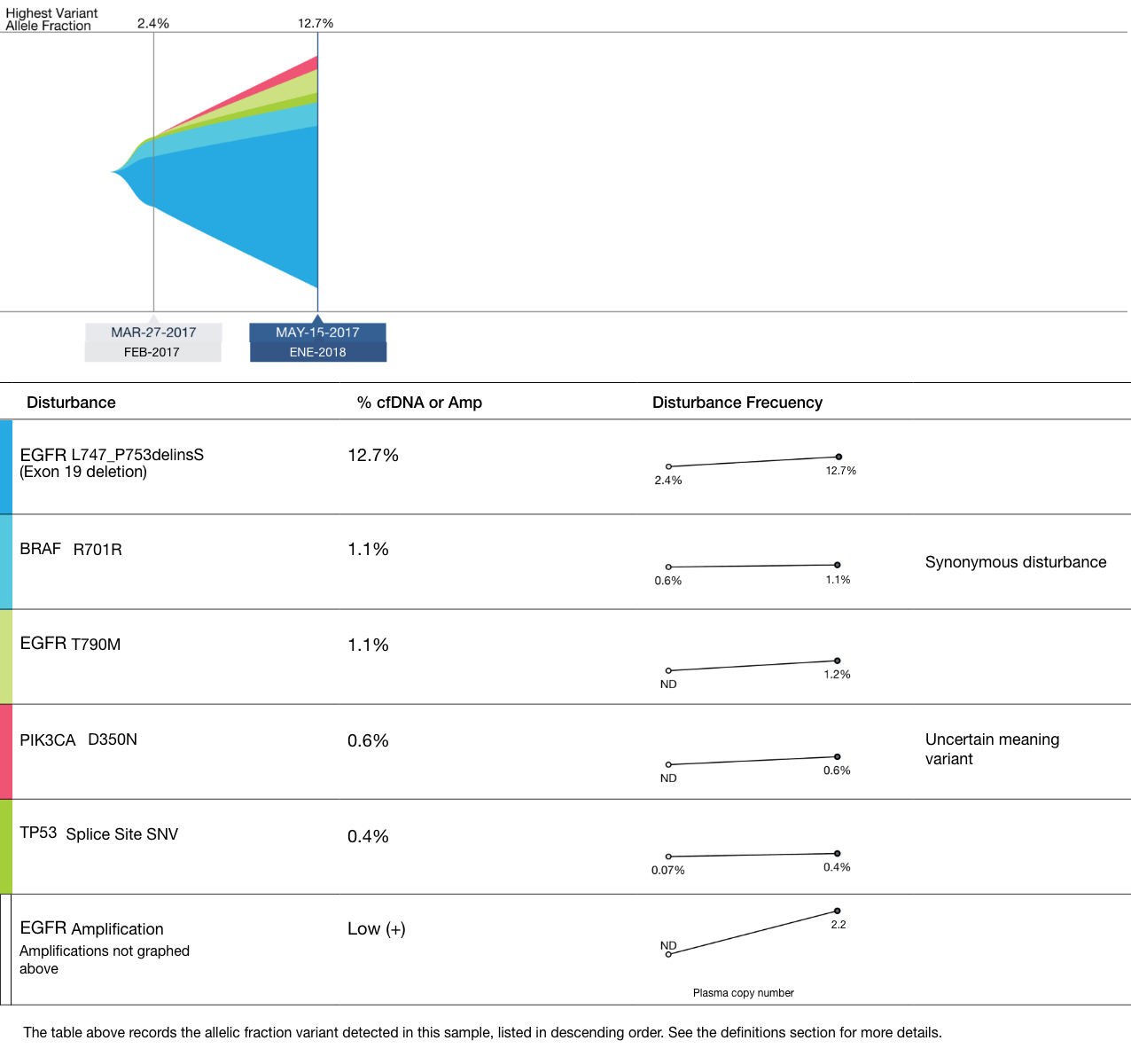
In advanced metastatic cancer, circulating tumor DNA (ctDNA) analysis in blood, or liquid biopsy, offers a non-invasive alternative to obtain the tumor molecular profile and guide the selection of targeted therapies.
Follow-up or “serial” liquid biopsies allow evaluating responses to treatment, identification of genomic alterations secondary to treatment (resistance mutations) that may be the cause of disease progression and that would dictate a change in therapeutic regimen, early detection of disease recurrence at the molecular level, as well as the appearance of new mutations during the evolution of the disease. Monitoring the amount of ctDNA may in turn reflect the response to treatment.
Liquid biopsy, unlike molecular analysis in tumor tissue, can capture genomic alterations from different metastases. That is, it can encompass the heterogeneity of the disease.
Genetic tests for the diagnosis of hereditary cancer
Unlike the acquired or somatic mutations in sporadic cancer, hereditary cancer is caused by germline (inheritable) mutations that can be passed from generation to generation. The test is usually done on blood samples.
Depending on the specific mutation, the risk of developing certain types of cancer can be determined in patients and their families, allowing multidisciplinary strategies for prevention or early detection and timely treatment of these tumors. Identification of germline mutations in certain genes can predict cancer behavior and/or response to certain targeted therapies.

Cancer Pathology
Our pathologists are an integral part of the multidisciplinary oncology team. The information they provide when performing the histopathological evaluation which includes the specific type of cancer, its degree of differentiation, size, its level of invasion, presence, or absence of vascular, perineural, and adjacent organs invasion, number of nodes with and without metastases, the evaluation of the surgical edges, and the pathological staging, is essential for making therapeutic decisions.
In patients who have received neoadjuvant therapy, that is, therapy (generally chemotherapy) prior to surgery, the pathologist evaluates response to treatment, reporting whether there is a residual viable tumor and its percentage.
In situations where there are previous samples, they are compared with the current sample to determine if the tumor has advanced histologically, and to distinguish between a metastasis or a second primary.
During surgical procedures, the oncological surgeon may require an intraoperative study by freezing, through which the pathologist provides relevant information that guides the most indicated surgical approach. The surgeon can send the pathologist a biopsy to determine if a tumor is benign or malignant, can send surgical borders to ensure that they are free of tumor, or samples of the tumor and ensure that they are representative and sufficient to reach a definitive diagnosis in the paraffin sections.
They also perform cytopathological diagnostics, or cell morphological analysis, on exfoliated cells or cells obtained from body fluids and fine needle aspirations.
We have a growing number of immunohistochemical markers to achieve more precise classifications of tumor types and subtypes, and to detect the presence of micrometastases in lymph nodes, among other clinical applications. Our Molecular Pathology Laboratory performs tests, such as PCR (polymerase chain reaction) and FISH (fluorescent in situ hybridization), of diagnostic, prognostic, and therapeutic relevance, through the detection of molecular targets.
When the oncologist requests more advanced molecular tests, such as next-generation sequencing, our pathologists ensure that the sample that is sent to the appropriate laboratory is optimal to obtain the most reliable result.

Cancer Pathology
Our pathologists are an integral part of the multidisciplinary oncology team. The information they provide when performing the histopathological evaluation which includes the specific type of cancer, its degree of differentiation, size, its level of invasion, presence, or absence of vascular, perineural, and adjacent organs invasion, number of nodes with and without metastases, the evaluation of the surgical edges, and the pathological staging, is essential for making therapeutic decisions.
In patients who have received neoadjuvant therapy, that is, therapy (generally chemotherapy) prior to surgery, the pathologist evaluates response to treatment, reporting whether there is a residual viable tumor and its percentage.
In situations where there are previous samples, they are compared with the current sample to determine if the tumor has advanced histologically, and to distinguish between a metastasis or a second primary.
During surgical procedures, the oncological surgeon may require an intraoperative study by freezing, through which the pathologist provides relevant information that guides the most indicated surgical approach. The surgeon can send the pathologist a biopsy to determine if a tumor is benign or malignant, can send surgical borders to ensure that they are free of tumor, or samples of the tumor and ensure that they are representative and sufficient to reach a definitive diagnosis in the paraffin sections.
They also perform cytopathological diagnostics, or cell morphological analysis, on exfoliated cells or cells obtained from body fluids and fine needle aspirations.
We have a growing number of immunohistochemical markers to achieve more precise classifications of tumor types and subtypes, and to detect the presence of micrometastases in lymph nodes, among other clinical applications. Our Molecular Pathology Laboratory performs tests, such as PCR (polymerase chain reaction) and FISH (fluorescent in situ hybridization), of diagnostic, prognostic, and therapeutic relevance, through the detection of molecular targets.
When the oncologist requests more advanced molecular tests, such as next-generation sequencing, our pathologists ensure that the sample that is sent to the appropriate laboratory is optimal to obtain the most reliable result.
Our Locations
At ABC Medical Center, we are prepared to serve you in out two Campuses 24/24h, 7 days a week.
Campus Observatorio
Sur 136 No. 116, Col. Las Américas,
Álvaro Obregón, 01120, Cd. de México.
Tel. 55 5230 8000
Campus Santa Fe
Av. Carlos Graef Fernández 154, Col. Santa Fe,
Cuajimalpa, 05300, Cd. de México.
Tel. 55 1103 1600