Contact us
Precision Medicine
-
Healthcare Professionals
Healthcare Professionals
Credentialing Requirements
- About ABC
-
Inclusive Health
- ABC Talent
- ABC Foundation I.A.P
- Contact
- ES
What is Intestinal Ischemia?
4 November 2025
Intestinal or mesenteric ischemia is a condition with a high mortality rate (up to 80%) that consists of the obstruction of blood circulation in the small intestine due to arterial narrowing or blockage, which can lead to irreversible intestinal damage.
When the affected blood circulation occurs abruptly, it is called acute mesenteric ischemia. This is caused by a blood clot, usually from the heart, and requires emergency surgical intervention.
On the other hand, chronic mesenteric ischemia develops progressively over a long period due to arterial narrowing caused by the accumulation of plaque on the artery walls. It is usually treated with open surgery or angioplasty.
Signs and symptoms Intestinal Ischemia
Symptoms vary depending on the type of mesenteric ischemia:
Acute Mesenteric Ischemia
Acute mesenteric ischemia usually presents with sudden and severe abdominal pain that is often disproportionate to the physical findings on examination.
Other common symptoms include nausea, vomiting, diarrhea, or bloody stools. In advanced stages, signs of sepsis or shock may appear.
This condition is a medical emergency because the sudden interruption of intestinal blood flow can cause necrosis of the intestine within a few hours if not treated promptly.
The acute form of the disease can lead to severe complications that can be fatal if not treated in time, such as:
- Septicemia: The release of chemicals into the blood to fight an infection, causing widespread inflammation that leads to organ failure.
- Permanent intestinal damage: The lack of blood circulation causes the death of tissue (necrosis) in the intestinal areas without blood supply.
Chronic Mesenteric Ischemia
In its chronic form, symptoms usually develop progressively. The main symptom is crampy abdominal pain that typically appears after eating, known as intestinal angina. This leads the patient to avoid eating for fear of pain, causing significant weight loss.
It’s also possible to have a feeling of bloating, nausea, or changes in bowel habits.
Even though the chronic form of intestinal ischemia is less urgent than the acute form, it also requires medical attention because it can progress to acute ischemia.
Diagnosis Intestinal Ischemia
Diagnosing intestinal or mesenteric ischemia requires a high degree of clinical suspicion, especially in patients with risk factors such as cardiovascular disease, atrial fibrillation, heart failure, or a history of thrombosis.
For acute ischemia, clinical findings such as severe abdominal pain and a lack of other physical signs, along with abnormalities in lab tests like leukocytosis, metabolic acidosis, or elevated lactate, can point to the diagnosis. However, these data are nonspecific and must be supplemented with imaging studies.
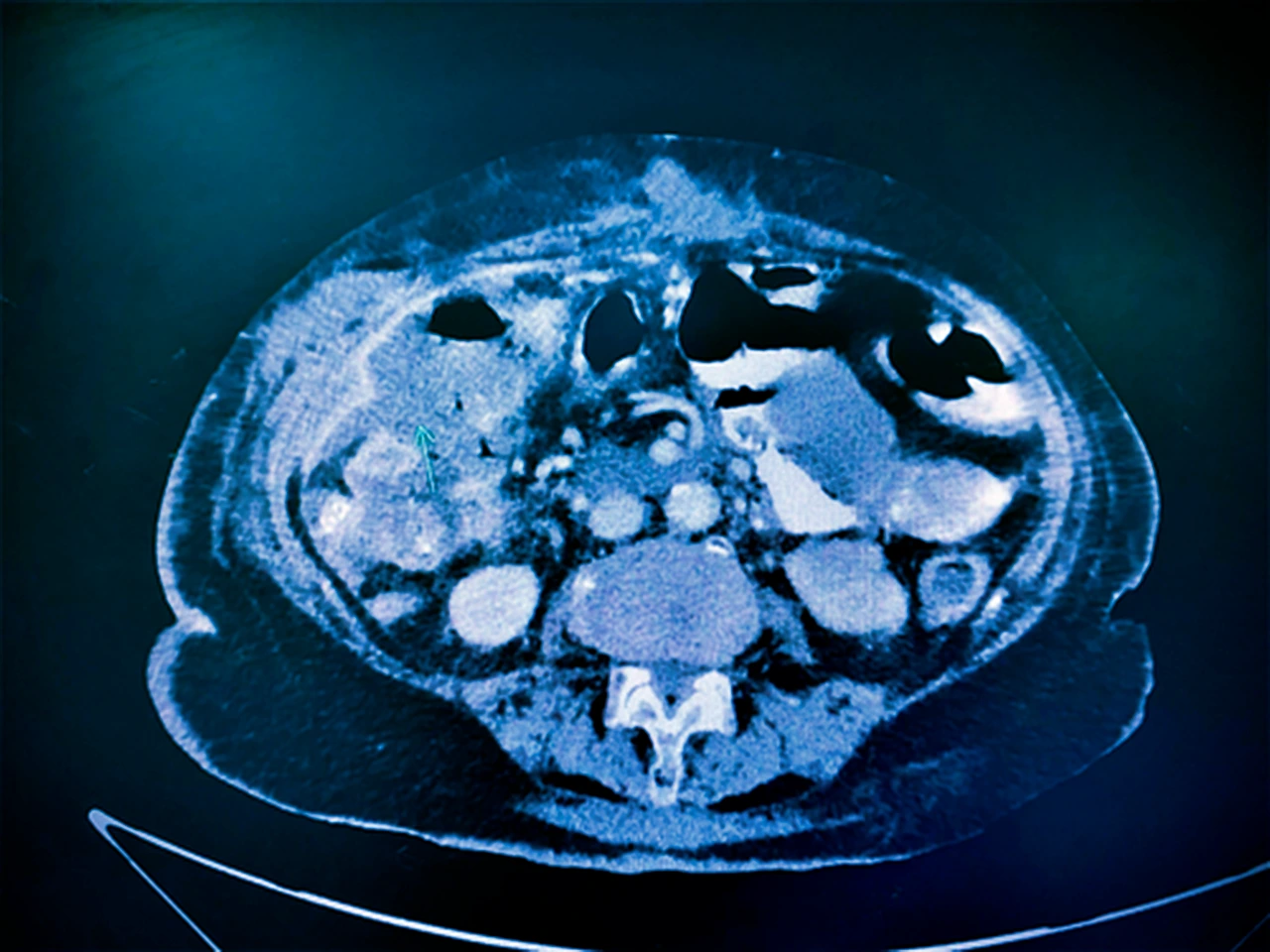
The preferred study is usually a CT angiogram with contrast, which allows for a detailed visualization of the mesenteric arteries and can detect occlusions, stenosis, or signs of intestinal damage.
In some cases, conventional mesenteric angiography may be used to both confirm the diagnosis and perform endovascular treatment.
For chronic ischemia, the findings usually include severe stenosis in at least two major mesenteric arteries, and the evaluation is typically done in patients with persistent postprandial symptoms.
Treatment Intestinal Ischemia
Acute intestinal ischemia is a medical emergency that requires immediate treatment to restore intestinal blood flow and prevent intestinal necrosis. Treatment will vary depending on the cause and may include anticoagulation, thrombolysis, angioplasty, or open surgery to remove clots, repair affected vessels, and resect necrotic intestinal segments.
Intensive supportive measures must also be initiated, such as intravenous fluids, pain management, correction of metabolic disturbances, and, in cases of sepsis, broad-spectrum antibiotics. The prognosis improves significantly if treatment is started within the first few hours.
For chronic intestinal ischemia, treatment is usually planned and focuses on restoring blood flow through vascular interventions like angioplasty with stent placement or revascularization surgery.
These options are considered in symptomatic patients, especially if there is persistent weight loss and postprandial pain.
At the same time, it is essential to control cardiovascular risk factors such as hypertension, dyslipidemia, and diabetes.
Timely treatment not only improves symptoms but also prevents progression to acute ischemia.
At ABC Medical Center’s Vascular, Arterial, and Venous Disease department, we can provide you with specialized care. Contact us!
Fuentes:
How can we help you?

Ricardo Ostos
Content CreatorRicardo can convey complex medical information in an accessible and friendly way so that all of our patients can understand and benefit from it. In addition, he has an empathetic approach, offering information and practical advice that really makes a difference in people's lives. #lifebringsustogether.
Learn more about Ricardo on LinkedIn
Pay in interest-free monthly installments in Specialty Centers, Check Ups, Diagnostic Tests, and Hospitalization
Get from 3 to 9 interest-free installments* with American Express or 6 installments* when paying with Banamex, BBVA, HSBC, Santander or 12 installments*
when paying with Banamex.
Privacy Overview
Error: Contact form not found.
We help you
Send us your request and we will forward it to our specialists. We will get in touch with you very soon.
If you have preferred times to receive our call, please indicate them in your message.
Thank you for contacting us!
Interest-free
months in:
Interest-free
months in:
Specialty Centers
Diagnostic Studies
Check-ups
Hospitalization1
Choose from3 to 9 months when paying with American Express cards 2. Or
6 months when paying with your credit card3 Banamex, BBVA Bancomer, HSBC, Santander.
Or 12 months exclusively when paying with Banamex3
Valid until December 31, 2025. Promotions not cumulative. Subject to restrictions 1. In hospitalization, medical fees are not included. 2. Minimum amount: $1,500 for 3 to 6 months and $3,000 for 7 to 9 months 3. Minimum amount $1,500. (Cards issued abroad are not eligible).
Comparison of COVID-19 vaccines
Pfizer-
BioNTech
Pfizer-BioNTech
What is its effectiveness and what does it refer to?
Vaccine type: mRNA
Effectiveness: 95% after the second dose in the prevention of symptomatic COVID-19.
No Does not contain egg, latex, or preservatives.
How many doses are needed?
Two doses are needed, at least 21 days apart (or up to six weeks apart, if necessary).
Who should or shouldn’t get the vaccine?
People who should receive the vaccine are those over 16 years old.
People who should not receive the vaccine are those who have a history of anaphylactic shock (severe allergy) or who are allergic to any component of this vaccine such as polyethylene glycol (PEG) or polysorbate.
What are the possible side effects of the vaccine?
Pain where the injection was given, fatigue, headache, muscle pain, chills, joint pain, fever, nausea, malaise, and swollen lymph nodes.
How long will it take for me to be protected and what does it protect me from?
After 14 days of having the complete scheme (after the administration of the 2nd dose), the protection period is still under study. It protects us from serious COVID-19 or requiring hospitalization.
Moderna
What is its effectiveness and what does it refer to?
Vaccine type: mRNA
Effectiveness: 94.5% after the second dose in the prevention of symptomatic COVID-19.
Does not contain egg, latex, or preservatives.
How many doses are needed?
Two doses are needed, at least 28 days apart (or up to six weeks apart, if necessary).
Who should or shouldn’t get the vaccine?
People who should receive the vaccine are those over 18 years old.
People who should not receive the vaccine are those who have a history of anaphylactic shock (severe allergy) or who are allergic to any component of this vaccine.
What are the possible side effects of the vaccine?
Pain where the injection was given, fatigue, headache, muscle pain, chills, joint pain, fever, nausea, and swollen lymph nodes in the arm in which you received the injection.
How long will it take for me to be protected and what does it protect me from?
After 14 days of having the complete scheme (after the administration of the 2nd dose), the protection period is still under study. It protects us from serious COVID-19 or requiring hospitalization.
Janssen/
Johnson
& Johnson
Janssen/ Johnson & Johnson
What is its effectiveness and what does it refer to?
Vector-based vaccine.
Effectiveness: 72.0% in the prevention of symptomatic COVID-19.
85% in the prevention of severe COVID-19.
Does not contain egg, latex, or preservatives./strong>
How many doses are needed?
Only one dose in needed.
Who should or shouldn’t get the vaccine?
People who should receive the vaccine are those over 18 years old.
People who should not receive the vaccine are those who have a history of anaphylactic shock (severe allergy) or who are allergic to any component of this vaccine.
What are the possible side effects of the vaccine?
Pain where the injection was given, headache, fatigue, muscle pain, chills, fever, and nausea.
How long will it take for me to be protected and what does it protect me from?
After 28 days of having the complete scheme (the last dose applied), the protection period is still under study. It protects us from 85% serious COVID-19 or requiring hospitalization.
AstraZeneca
and
Oxford
University
AstraZeneca and Oxford University
What is its effectiveness and what does it refer to?
Adenovirus vector-based vaccine.
Effectiveness: 82% after the second dose in the prevention of symptomatic COVID-19.
How many doses are needed?
Two doses are needed, at least 56 days apart (or up to 84 days apart, if necessary).
Who should or shouldn’t get the vaccine?
People who should receive the vaccine are those over 18 years old.
People who should not receive the vaccine are those who have a history of anaphylactic shock (severe allergy) or who are allergic to any component of this vaccine.
What are the possible side effects of the vaccine?
Pain where the injection was given, fatigue, headache, myalgia, arthralgia, and fever, which were mild to moderate in intensity and disappeared within 48 hours of vaccination.
How long will it take for me to be protected and what does it protect me from?
After 14 days of having the complete scheme (after the administration of the 2nd dose), the protection period is still under study. It protects us from serious COVID-19 or requiring hospitalization.
Sputnik V
What is its effectiveness and what does it refer to?
Adenovirus vector-based vaccine.
Effectiveness: 92% after the second dose in the prevention of symptomatic COVID-19.
How many doses are needed?
Two doses are needed, at least 21 days apart (or up to six weeks apart, if necessary).
Who should or shouldn’t get the vaccine?
People who should receive the vaccine are those over 18 years old.
People who should not receive the vaccine are those who have a history of anaphylactic shock (severe allergy) or who are allergic to any component of this vaccine.
What are the possible side effects of the vaccine?
Pain where the injection was given, fatigue, headache, myalgia, arthralgia, and fever, which were mild to moderate in intensity and disappeared within 48 hours of vaccination.
How long will it take for me to be protected and what does it protect me from?
After 14 days of having the complete scheme (after the administration of the 2nd dose), the protection period is still under study. It protects us from serious COVID-19 or requiring hospitalization.
Anti-Herpes Zoster
Herpes zoster is a painful, burning rash. It usually appears on one part of the body and can last for several weeks. It can cause long-lasting severe pain and scarring. Bacterial skin infections, weakness, muscle paralysis, hearing or vision loss may occur less frequently. Herpes zoster is caused by the same virus that causes chickenpox. After you have had chickenpox, the virus that caused it remains in the body of nerve cells. Sometimes after many years, the virus becomes active again and causes herpes zoster.
Vaccination is indicated in the following cases:
- Immunization of patients from 50 years of age for the prevention of herpes zoster and post-herpetic neuralgia (PHN), reduce pain associated with acute or chronic herpes zoster.
Scheme type:
- Single dose.
Rabies
Human rabies is a viral disease transmitted by the bite of an infected animal. It is characterized by acute encephalomyelitis (an aggressive response of the immune system that destroys the myelin layer of the nerves and alters its function at the level of the brain or spinal cord).
Vaccination is indicated in the following cases:
- Prevention of rabies in subjects exposed to risk of contamination. It is recommended for certain international travelers, based on the occurrence of animal rabies in the destination country.
Scheme type:
There are two types.
1. Pre-exposure scheme, consists of three doses of rabies vaccine:
- First dose, on the chosen date.
- Second dose 7 days after the first dose.
- Third dose 28 days after the first dose.
2. Post-exposure scheme, people not vaccinated against rabies, consists of five doses of rabies vaccine.
- First dose, on the date indicated.
- Second dose 3 days after the first dose.
- Third dose 7 days after the first dose.
- Fourth dose 14 days after the first dose.
- Fifth dose 28 days after the first dose.
* If the individual continues to be at risk of exposure to the disease, revaccination should be considered.
Pneumococcal vaccines
Pneumococcal disease can cause serious infections in the lungs (pneumonia), the bloodstream (bacteremia), and the lining of the brain and spinal cord (meningitis).
Two vaccines help prevent pneumococcal disease:
- Pneumoconjugate 13 (pneumococcal conjugate vaccine)
- Pneumococcal 23 (pneumococcal polysaccharide vaccine)
Vaccination is indicated in the following cases:
- Active immunization for the prevention of invasive disease caused by Streptococcus pneumoniae in adults 65 years of age and older.
Scheme type:
- *Two pneumococcal vaccines are recommended for all adults 65 years of age or older.
*One dose of Pneumococcal 13 vaccine should be given first, followed by one dose of Pneumococcal 23 vaccine, depending on your age and health.
